战伤统计分析
02-What Ukraine’s bloody battlefield is teaching medics
05-大规模伤亡事件对医生和护士焦虑、抑郁和创伤后应激障碍的影响——一项系统审查方案。
01-Decision Support System Proposal for Medical Evacuations in Military Operations
01-军事行动中医疗后送的决策支持系统建议_1_23_translate
03-983例平民爆炸和弹道伤亡分析及伤害负担模板的生成——一项观察性研究
04-Characterization of Female US Marine Recruits- Workload, Caloric Expenditure, Fitness, Injury Rates, and Menstrual Cycle Disruption during Bootcamp
03-Analysis of 983 civilian blast and ballistic casualties and the generation of a template of injury burden- An observational study
04-美国海军陆战队女性新兵的特征——训练期间的工作量、热量消耗、体能、受伤率和月经周期中断
08-在救援现场,受害者周围环境的3D模型生成
07--估计冲突损失和报告偏差
06-EGFA-NAS- a neural architecture search method based on explosion gravitation field algorithm
05-Effects of mass casualty incidents on anxiety, depression and PTSD among doctors and nurses- a systematic review protocol.
06-EGFA-NAS——一种基于爆炸引力场算法的神经结构搜索方法
07-Estimating conflict losses and reporting biases
09-新技术应用中的精益方法——院前紧急医疗服务的风险、态势感知和复原力整合
08-Generation of 3D models of victims within their surroundings at rescue sites
10-胸腹枪伤的处理——来自南非一个主要创伤中心的经验
09-Lean approach in the application of new technologies- integration of risk, situational awareness, and resilience by a prehospital emergency medical service
10-Management of thoracoabdominal gunshot wounds – Experience from a major trauma centre in South Africa
02-乌克兰血腥的战场教给医护人员的是什么_1_1_translate
士兵跳伞造成骨科损伤的描述性研究
美国陆军部队类型的肌肉骨骼损伤发生率:一项前瞻性队列研究
军事静线空降作战中受伤的危险因素:系统回顾和荟萃分析
战伤数据库研究进展与启示
从角色2到角色3医疗设施期间战斗人员伤亡管理
美军联合创伤系统应用进展及其对我军战伤救治的启示
2014-2020年俄乌战争混合时期作战伤员膨胀子弹致结肠枪伤
关于“2001-2013年军事行动中的战斗创伤教训”的联合创伤系统更新 英文05 Joint Trauma System
创伤与伤害小组委员会 剧院创伤经验教训 英文 Theater_Trauma_Lessons_Learned
创伤和伤害小组委员会战区创伤经验教训 英文 111813Trauma and Injury Update on Theater Trauma Lessons Learned
向国防卫生委员会提交的关于“2001-2013年军事行动中的战斗创伤教训”的联合创伤系统更新 2016/8/9
战斗伤亡护理研究计划 会议材料 -
-
+
首页
2014-2020年俄乌战争混合时期作战伤员膨胀子弹致结肠枪伤
古梅纽克等人。*BMC手术(2023)23:23* <https://doi.org/10.1186/s12893-023-01919-6> BMC手术 **研究** **开放访问** 2014-2020年俄乌战争混合时期受伤的战斗  病人被扩大子弹击中结肠 科斯蒂安蒂恩古梅纽克1,2,Igor A。卢林3,4,Ievgen Tsema5, Lesia Malynovska5, Maksym戈罗贝科6和安德里的晚餐6* **摘要** **背景:结肠枪伤是武装疾病的常见损伤。**高能现代武器的一个例子是空心子弹,它与增加的组织损伤和致 命的结果有关。本研究的目的是评估战斗患者的结肠枪伤,并评估空心点子弹与形状稳定子弹对结肠损伤 患者的临床特征的差异。 患者和方法对2014年至2020年乌克兰东部374名腹部枪伤的男性士兵进行临床资料分析。374例受伤患者中 , 112例(29.9%)被诊断为穿透性枪伤: 69/112例(61.6%)被形状稳定的子弹伤害,空心点子弹受伤 43/112例(38.4%)。 结果空心子弹伤患者失血性休克分期较严重,III-IV期休克25例(58例。1%)被空心子弹伤害的病人和。17 例(24.6%)患者被形状稳定的子弹损伤(p = 0.0004)。与右侧结肠或横结肠相比,左侧结肠损伤更频繁 : 21例(48.8%)患者被空心子弹损伤(p <0.0001),41例(59.4%)患者形状稳定子弹损伤(p = 0.032 ) 。在整个队列中,中结肠的频繁损伤存在明显的差异(p = 0.023)。空心子弹伤的患者出现3-5个区域 的结肠枪击缺损,在18例(41.8%)空心子弹伤的患者中发现,没有形状稳定的子弹损伤(p = 0.0001)。 7例(16.3%)空心子弹损伤患者结肠损伤评分(CIS)IV,2例形状稳定子弹损伤患者结肠损伤评分(2.9% ) (p=0.011)。对14例(69%)形状稳定子弹损伤患者和12例(27.9%)空心子弹损伤患者进行了结肠造口 术(p > 0.05)。15例(35%)患者在空心子弹损伤后死亡,而9例(13%)患者在形状稳定的子弹损伤后死 亡(p = 0.0089)。 **结论所有患者如有腹部穿透性损伤(无出口伤口),应怀疑有子弹扩张损伤,并仔细进行腹部翻修,确** **定可能的多器官损伤及肠多枪缺损。** *Correspondence: 安德里的晚餐 andrii.dinets@knu.ua 完整的作者信息列表可在文章的末尾获得  ©作者(s) 2023。开放获取本文授权在知识共享署名4.0国际许可,允许使用、共享、适应、分布和复制在任何媒体 或格式,只要你给适当的信贷原作者(s)和来源,提供一个链接到知识共享许可,并表明如果有变化。本文中的图片 或其他第三方材料都包含在文章的知识共享许可中,除非在材料的信用额度中另有说明。如果材料没有包含在文章 的知识共享许可中,并且您的预期使用不被法律法规允许或超过了允许的使用,您将需要直接获得版权所有者的许 可。若要查看此许可证的副本,请访问http://creativecommons.org/licenses/by/4.0/。知识共享公共领域奉献豁 免。org/publicdomain/zero/1.0/)适用于本文中提供的数据,除非在该数据的信用额度中另有说明。 古梅纽克等人。*BMC手术* *(2023)* *23:23* 第2页共9 页 关键词结肠受伤,枪击,乌克兰战争,形状稳定的子弹,空心点子弹,膨胀的子弹 **介绍** 结肠的枪伤是武装武器中常见的损伤, 由于现代高能量 武器[1,2]的损伤特性增加,这与战斗人员的严重创伤有 关。这种枪伤可能对软组织和内脏器官造成巨大的损伤 , 导致致命的结果或更延长的治疗和康复时间[3,4]。乌 克兰战争始于2014年,在前8年里,这场战争作为混合战 争进行,随后在2022年两军开始直接瞄准[5,6]。在2014 -2020年的混合时期,我们注意到俄罗斯军队经常使用各 种具有高破坏属性的武器(e。*g.*空心子弹),这是国际法 禁止的[7]。考虑到这一事实,乌克兰的军事医务人员提 出了这样一个问题:上述类型的子弹是否会影响枪伤的 严重程度和伤害的具体位置,以及与病人的生存及其治 疗的关系。这些结果被用于更新临床指南,并在适当的 级别升级军事医院,以便准备在使用被禁止的高能量武 器时提供援助。在本研究中,我们重点分析了上述情况 下的结肠损伤。乌克兰的军事医生受到了对被现代高能 量武器伤害并遭受严重腹部创伤的军事人员的管理和康 复方面的挑战。这种现代武器的一个例子是空心子弹, 它是一种特殊形状的子弹,在撞击目标并对软组织和内 部器官造成严重伤害时,会膨胀成多个较小的炮弹。特 空心点子弹可以穿孔高级防弹衣[8,9]。这种弹道特性可 能与严重的腹部创伤有关:多器官损伤、肠多穿孔伴大 量粪便转移,以及失血性休克和腹膜后血肿[10,11]伴出 血的高风险。空心点子弹的弹道特性也与结肠壁的多个 全层枪伤缺陷有关,而结肠壁的单一缺陷是罕见的[8,12] 。 这种空心子弹的枪伤可能与对抗病人的致命结果有关 , 即使是关于“黄金时间 ”和损害控制手术的原则。空 心子弹的弹道特征设想在撞击时扩大,然后分布多个碎 片或子弹迅速出现, 对组织造成更大的损害。利用这些特征,x射线成为检测 腹部金属碎片和建立损伤机制的有效工具。关于乌克兰 战争中结肠的枪伤,我们知之甚少。本研究的目的是评 估战斗患者的结肠枪伤,并评估空心点子弹与形状稳定 子弹对结肠损伤患者的临床特征的差异。 **材料和患者** 2014年至2020年期间,乌克兰武装部队在乌克兰东部腹 部枪伤和结肠受伤的士兵都有资格参加这项回顾性研究 。在本研究中,我们假设空心点子弹枪伤患者与形状稳 定子弹枪伤患者具有不同的临床特征和结果。对患者进 行了关于子弹类型的评估,并取决于是否有碎片化的空 心点子弹和碎片化的子弹。形状稳定的子弹。在被爆炸 性弹药(火炮、地雷、手榴弹等)伤害时,患者不被纳 入研究。研究人员确认了374名男性患者,他们在位于距 离前线20公里区域的一家军事基地医院(二级医疗护理 ) 接受了手术治疗。在乌克兰国家军事学说中使用了“ 级别 ”一词, 旨在显示提供医疗援助的fve层的分层。每 一级都是一种医疗级别,从1到5逐步组织,应用治疗、 疏散、病人的特殊支持和康复。第一级是急救,在疏散 期间或受伤时组织。二级医院对应于陆军战场医院,住 院床位有限,距离前线20-40公里。二级医院设有腹腔镜 检查。三级是专门的医疗和外科护理,在一家大型医院 提供,位于哈尔科夫、德尼普罗、奥德萨、文尼西亚、 基辅等城市,那里有先进的设备(CT、MRI等)。还有高 技能的外科医生。IV级是战场菲尔德区以外的一层高度 专业化的医疗援助,为需要更长时间治疗或需要较低 II/III级医疗能力不足的患者提供高科技医疗设备的应 用。第五级是一级的康复设施。 古梅纽克等人。*BMC手术* *(2023)* *23:23* 第3页共9 页 在374例结肠枪伤患者中,112例(29.9%)穿透性枪伤 患者纳入研究组,而262例(70.1%)患者因弹片伤导致 穿透性枪伤未纳入研究组。在研究组的112例患者中,69 例(61.6%)被形状稳定的子弹伤害,43例(38.4%)患 者受伤。在“黄金时间 ”的[13]时间内,将受伤的患者 从战场上撤离。 所有患者都接受了二级医疗援助。在二级医院入院时 , 所有患者均被诊断为枪伤和失血性休克,需要在重症 监护病房(ICU)进行复苏。休克的严重程度是根据美国 外科医生学会高级创伤生命支持系统(ATLS)来确定的 。所有患者均采用损伤控制策略。根据结肠损伤量表(C IS)对结肠损伤进行评估。 二级没有计算机断层扫描。应用腹部x射线检测弹丸的 定位或其碎片的方向(翻滚)、变形和碎片(碎片的数 量和碎片扩散的面积)。 右结肠部分构成盲肠、升结肠和肝弯曲。左结肠部分 形成脾结肠弯曲、降结和乙状结肠。作为上结肠,我们 考虑了横结肠、肝和脾弯曲、中结肠-升结肠和降结肠, 以及下结肠-盲肠和乙状结肠。 **统计分析** 使用SPSS v(IBM,USA)软件进行统计分析。.22卡方测 试(χ2-检验)用于检验分类值的零假设,而连续变量采 用学生t检验和单因素方差分析。p<为0.05,认为差异有 统计学意义。 **结果** 所有患者的平均年龄为24.7岁(范围为19-47岁)。82例 (73.2%)患者在受伤至入院的1小时内(平均时间55.3 ± 1.17 min)撤离至二级,符合“黄金时间 ”的原则。 数据分析结果见下表。详细的统计数据见附加fle 1: 表S1,附加fle 2:表S2,附加fle 3:表S3。对失血性 休克分期的分析见表1和附加fle 1:表S1。18例(41.9% ) 空心子弹损伤的患者出现失血性休克III期,比13例 ( 18.8%)形状稳定子弹损伤的患者更常见(p = 0.0081) 。相比之下,2例(4.7%)空心子弹损伤患者被诊断为失 血性休克I期,相比25例(36.2%)形状稳定子弹损伤患 者的发生率较低(p = 0.0001)。52例(75.4%)形状稳 定子弹损伤患者出现I-II期休克,18例(41.9%)(p=0. 0004)。 在剖腹手术或腹腔镜检查中,所有112例(100%)患者 都被诊断为各种结肠壁损伤的定位(表2,图。1, 2).数 据分析显示,21例(48.8%)空心子弹伤(p <0.0001) 和41例(59.4%)患者的左结肠部位比右结肠或横结肠伤 更常见。数据分析显示,80例(71.4%)患者被诊断为左 侧和中结肠枪伤。 对整个队列的分析显示,65例(58%)患者结肠多发损 伤,而47例(42%)患者发现单一结肠枪伤(表3) 。43 例(100%)空心子弹损伤患者结肠有多个伤口(2例或2 个以上缺陷),是22例(31.8%)的患者的3倍(p = 0.0488) 。此外,18例(41.8%)患者在空心子弹的损伤 下表现出更高频率的3-5个缺陷 表1形状稳定或空心子弹枪伤与失血性休克严重程度的分析 **冲击严重程度** **患者分组** **所有患者n.=112** **p值** **被形状稳定的子弹伤害** **,** **n** **=** **69** **被空心点子弹受伤n** **=** **43** 阶段 I 25 (36.2%) 2 (4.7%) II 27 (39.1%) (37.2%) III 13 (18.8%) 18 (41.9%) IV 4 (5.8%) 7 (16.3%) 16 27 43 31 11 (24.1%) (38.4%) (27.7%) (9.8%) 0 0 0.000 1.838 9.008 1 0.0699 古梅纽克等人。*BMC手术* *(2023)* *23:23* 第4页共9 页 表2用形状稳定或空心点子弹定位枪伤缺陷进行的结肠损伤分析 **结肠参数** **患者分组** **所有患者n.=112** **p值** **被形状稳定的子弹伤害** **,** **n** **=** **69** **被空心点子弹受伤n** **43** **=** 结肠部位 盲肠 6 (8.7%) 2 (4.7%) 升结肠 9 (13.0%) 9 (20.9%) 18 (16.1%) 0.27 肝性性疲劳 3 (4.3%) 4 (9.3%) 7 (6.3%) 0.29 横结肠 10 (14.5%) 7 (16.3%) 17 (15.2%) 0.80 脾脏 5 (7.2%) 1 (2.3%) 6 (5.4%) 0.26 下结肠 21 (30.4%) 12 (27.9%) 33 (29.5%) 0.78 乙状结肠 15 (21.7%) 8 (18.6%) 23 (20.5%) 0.69 每组结肠侧的p值比较 0.0005 0.0171 < 0.0001 右侧结肠 18 (26.1%) 15 (34.9%) 33 (29.5%) 0.32 横结肠 10 (14.5%) 7 (16.3%) 17 (15.2%) 0.80 左侧结肠 41 (59.4%) 21 (48.8%) 62 (55.4%) 0.27 每组结肠水平内的p值比较 < 0.0001 0.032 < 0.0001 上结肠 18 (26.1%) 12 (27.9%) 30 (26.8%) 0.83 中结肠 30 (43.5%) 21 (48.8%) 51 (45.5%) 0.58 下结肠 21 (30.4%) 10 (23.3%) 31 (27.7%) 0.41 各组内p值的比较与腹膜的关系 0.18 0.091 0.023 腹膜内的 39 (56.5%) 22 (51.2%) 61 (54.5%) 0.58 腹膜外的 30 (43.5%) 21 (48.8%) 51 (45.5%) 每一组内的p值比较 0.44 0.91 0.50 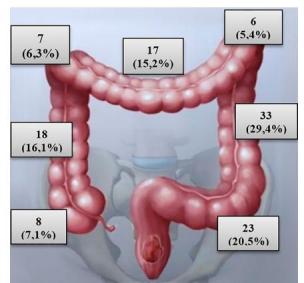**图**1.研究队列中结肠各部位的枪伤示意图 结肠壁,与无形状稳定的子弹损伤患者相比(p = 0.0001) 。4例(9.3%)空心子弹损伤患者发现结肠壁 ≥5缺陷的结肠伤口,但无形状稳定的子弹损伤患者(p = 0.0199)。 CIS分析报告见表4和附加fle 3:表S3。11例(25.6% ) 空心点子弹损伤患者发生CIS III的频率明显高于7例 形状稳定子弹损伤患者(10.1%)(p=0.031)。7例(16. 3%)空心子弹损伤患者检测到CIS IV,而2例(2.9%)形 状稳定子弹损伤患者检测到CISIV(p=0.011)。 x线片显示17例(24.6%)形状稳定的患者腹部有外来 金属密度物体,随后剖腹检查。3).在12 (27。9%)空心 子弹损伤患者7例(16.3%)患者发~现不同大小的多个子 弹碎片,13例(30.2%)患者发现6 10个碎片,11例(25. 6%)患者发现11-15个碎片。子弹碎片的腹部x射线例子 如图所示。3. 古梅纽克等人。*BMC手术* *(2023)* *23:23* 第5页共9 页 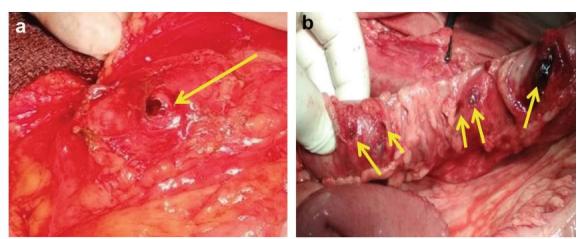**图**2例结肠枪伤的术中照片。结肠的一个伤口(有箭头标记的入口枪孔)。B子弹碎片造成结肠多重损伤(用箭头标记) 表3形状稳定或空心点子弹对结肠损伤的定位和枪击缺陷数量的分析 **结肠损伤部位** **患者分组** **被形状稳定的子弹伤害,n** **=** **69** **被空心点子弹受伤n** **=** **43** **结肠缺损数,n=** **2** **3** **–4** ≥ 5 **2** **3** **–4** ≥ 5 塞库姆,n= 0 0 0 1 1 0 上升结肠,n= 3 0 0 5 4 0 肝性疲劳,n= 2 0 0 3 1 0 横结肠,n= 1 0 0 2 4 1 脾脏,n= 3 0 0 0 1 0 降结肠,n= 4 0 0 7 3 2 乙状结肠,n= 9 0 0 3 4 1 合计 22* (31.8%) 0 0 21 (48.8%) 18 (41.8%)** 4 (9.3%)** * p值:*0.0488,**0.0001、***0.0199 表4结肠损伤量表分析结肠损伤与空心子弹或形状稳定子弹损伤的结肠损伤严重程度分析 **结肠损伤量表(CIS)** **因素** **患者分组** **所有受伤的n** **=** **112** **p值** **被形状稳定的子弹伤害** **,** **n** **=** **69** **被空心点子弹受伤n** **=** **43** CIS第一阶段 28 (40.6%) 0 (0.0%) 28 (25.0%) < 0.0001 微光 31 (44.9%) 23 (53.5%) 54 (48.2%) 0.38 罗马数字 3 7 (10.1%) 11 (25.6%) 18 (16.1%) 0.031 增值 2 (2.9%) 7 (16.3%) 9 (8.0%) 0.011 V 1 (1.4%) 2 (4.7%) 3 (2.7%) 0.31 蘑菇子弹(无花果。19例(44.2%)空心子弹损伤的患者 发现4),没有形状稳定子弹损伤的患者发现4)(p<0.000 1)。 表5总结了具体的操作列表。这一点在操作类型上没有 明显的差异 在研究小组中。对14例(20.3%)形状稳定子弹损伤患者 和12例(27.9%)空心子弹损伤患者进行了结肠造口术。 24例(21.4%)患者术后死亡。其中,15例(35%)患 者在受伤后死亡 古梅纽克等人。*BMC手术* *(2023)* *23:23* 第6页共9 页 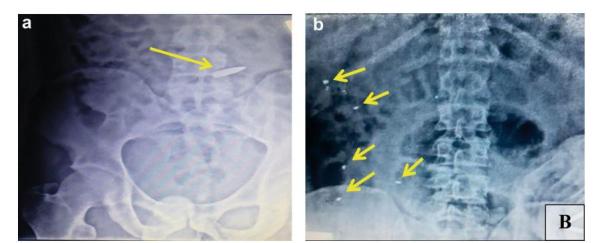**图**3x线照片显示腹部碎片的金属密度特征 **图**4术中照片显示空心子弹(外科医生手臂上的黄色金属物体) 空心子弹,而9例(13%)患者被形状稳定的子弹损伤后 (p =0.0089)。二级患者死亡的原因是大出血、心脏衰 竭和呼吸衰竭。III级死亡的原因是结直肠吻合口失败和 吻合口漏、腹膜炎和小肠消化性溃疡穿孔。四级死亡的 原因是脓毒症、腹部脓肿、化脓性肺炎和急性肠梗阻。 无法获得详细的后续数据,这是一个局限性。 **讨论** 这篇论文是第一项研究,报告了一个战斗队列的数据, 其中空心子弹已被用于对付乌克兰武装部队 自2014年以来。乌克兰战争与由于使用被禁止的武器, 包括空心子弹,对乌克兰武装部队造成的特殊结肠损伤 模式有关。这种违反与国际战争有关的法律的行为在以 前的文献中没有描述过。虽然北约标准通常用于个人身 体保护,使用战术头盔和模块化战术背心对颈部、胸部 、腹部和腹股沟的弹道保护,但我们的结果显示严重的 结肠损伤。考虑到修饰子弹的损害特性, 目前正在研究 开发更好的个人身体保护,但此类研究的细节已被分类 , 无法获得。这项研究强调了与传统形状稳定子弹相比 , 现代空心子弹损伤结肠损伤的各种临床结果。研究表 明,被空心子弹损伤的患者有严重的创伤,死亡率较高 。本研究揭示了枪伤结肠损伤的临床特点和处理方法, 这可能有助于民事和战斗伤亡人员的进一步临床应用。 与其他报道类似,我们发现大多数患者在“黄金时间 ” 内被疏散到II级,并按照损伤控制手术的原则进行治 疗。损伤控制手术是乌克兰军事医学的标准方案,与其 他关于腹部枪伤创伤的研究相一致[13-16]。 虽然我们还没有发现关于空心点子弹损伤vs。可变形 的子弹,来自这项研究的证据,以及其他内伤口弹道学 的实验研究,同意了我们关于这种武器[8,9,17,18]增加 组织损伤的数据。我们的fns表明,大多数患者同时有其 他器官损伤,支持上述假设。 古梅纽克等人。*BMC手术* *(2023)* *23:23* 第7页共9 页 表5研究队列中的外科手术情况分析 **操作类型** **形状稳定子弹n** **=** **69** **被空洞的子弹打伤** **n** **=** **43** 腹腔镜结肠伤口初次修复,n= 2 (3.0%) 0 结肠伤口初次修复,n= 3 (4.3%) 0 结肠创面一期修复+结肠造口术,n= 0 1 (2.3%) 结肠创面一期修复+小肠切除术,n= 21 (30.4%) 9 (20.9%) 结肠伤口一期修复+结肠造口术+输尿管伤口一期修复和输尿管支架植入术,n= 0 2 (4.6%) 结肠伤口一期修复+胆囊切除术,n= 3 (4.3%) 0 结肠创面一期修复,经造口+胃创面一期修复,n= 4 (5.8%) 2 (4.6%) 结肠伤口一期修复+脾切除术,n= 2 (3.0%) 2 (4.6%) 结肠创面修复修复+肝创面修复+结肠造口术,n= 3 (4.3%) 2 (4.6%) 结肠伤口一期修复+结肠造口术+胰腺伤口一期修复,n= 2 (3.0%) 0 Extraperitonization, n = 2 (3.0%) 0 右半结肠切除术,n= 2 (3.0%) 2 (4.6%) 右半结肠切除术+回肠造口术,n= 0 1 (2.3%) 右半结肠切除术+右肾切除术,n= 2 (3.0%) 5 (11.6%) 右半结肠切除术+肝伤口一期修复,n= 14 (20.0%) 5 (11.6%) 左半结肠切除术,n= 1 (1.4%) 0 左半结肠切除术+左肾切除术,n= 3 (4.3%) 8 (18.6%) 哈特曼手术,n= 1 (1.4%) 2 (4.6%) 哈特曼的手术+膀胱伤口初级修复,n= 4 (5.8%) 2 (4.6%) 与Busic等人的观点一致。和Elfaedy等人,我们也证 实了在我们的患者中失血性休克的高发生率,提示这些 枪击并发症是一种常见的事件[11,19]。此外,我们还发 现,被空心点子弹损伤的患者发生失血性休克的频率高 于形状稳定型子弹,这是现代武器造成严重创伤的另一 个证据。较高的休克严重程度与结肠组织的缺血和坏死 相关,从而增加细菌定植,导致吻合口泄漏或[11,20]失 败的风险更高。 与其他报道相似,与其他部位相比,左侧结肠(脾结 肠融合、降结肠和乙状结肠)和中结肠(中结肠、上、 降结肠)经常受伤[1、11、21-24]。值得注意的是,结 肠损伤与粪便转移的高风险有关。沃森等人。显示高能 弹对左侧结肠损伤患者粪便转移的风险较高。我们的研 究结果也显示了左侧结肠损伤的高频率,我们假设有这 种枪伤部位的患者有更高的并发症风险,需要进行结肠 造口术。然而,我们也建议将子弹类型(即空心子弹) 作为增加组织损伤的额外因素。我们的研究结果似乎表 明,损伤的机制是由 现代子弹可以影响所有的结肠部分,而与子弹类型无关 。 与在该领域进行的其他研究不同,我们发现58%的患者 结肠有多重损伤,这高于其他队列。例如,他等。显示 为12%,Steele等人。在非战斗创伤[21,23]的研究中, 诊断为结肠一次以上损伤的患者的多重损伤占15%。卡迪 等人。21.3%的[25]患者显示大肠和小肠的多节段损伤。 然而,我们的研究与Bothaig i等人一致,他们在腹部战 场创伤[22]的研究中发现56例患者有64例结肠直肠伤口 。这种差异可以用在我们的队列中经常应用空心子弹来 解释。 CIS分析显示,在整个队列中有48.2%的患者患有CIS II或更高版本。我们的观察结果与Fealk等人一致,报告 59%的患者患有CIS > 2,而Miller等人的平均CIS为2.4 [24,26]。在这项研究中,我们发现没有患者患有CIS I , 但与形状稳定的子弹相比,在空心子弹损伤的个体中 发生CIS III和IIV的频率更高。这些疫苗可能在因扩大 子弹而受伤的病人的管理中发挥重要作用 古梅纽克等人。*BMC手术* *(2023)* *23:23* 第8页共9 页 有关于子弹膨胀会导致严重的结肠创伤的证据。 在我们的队列中,总体的结肠造口率(20.3%)与其他 报道形成了对比: Steele(33%),格拉斯哥(36.3%) , Watson (36。9%),Oosthuizen等。(50%)或Mitchao 等人。 (2.5%) [1, 10, 15, 23, 27].卡迪等人。在粪便 高扩散或损伤控制手术[25]中,13.6%的结直肠伤口患者 进行了结肠造口术。从其他系列的分析和我们的经验来判 断,外科医生在每种情况下决定选择某种手术入路有多种 因素,包括结肠造口术。所观察到的结肠造口术的倾向可 能归因于严重的结肠创伤,这与之前发表的[15,16,21]系 列文章一致。我们同意其他研究人员的观点,避免结肠造 口,并通过[15,16,21]造口,对选定的受伤患者进行初次 闭合。然而,在本研究中,空心子弹造成的结肠损伤与更 严重的创伤相关,应在损伤控制手术的背景下进行腹部评 估后,决定进行结肠造口术。 枪伤结肠伤患者的死亡率通常很高,主要是由于多器 官损伤和严重的失血性休克[15]。在我们的研究中,我 们显示21.4%的患者有致命结局,这与乌氏等人的研究数 据接近,该等人显示总死亡率为26%,vertres等人的26% 。29%的枪伤患者为[11,16]。相比之下,埃尔菲迪等人 。显示死亡率为6。9%;然而,在该研究中,40%的患者 没有发生失血性休克,这是腹部枪伤死亡的患者,包括 结肠[11]的一个危险因素。格拉斯哥等。显示总死亡率 为9例。5% [10].钢铁等。显示战斗患者[23]的死亡率为 17.7%。Bothaig i等人证实,与结肠相关的死亡率为零。 Mitthue等人。 [22, 27].卡迪等人。死亡率为12.8%,失 血性休克是最常见的死亡原因。根据已发表的系列报道 , 据报道,多处枪伤的死亡率很高,本研究也显示了[28] 。 **结论** 综上所述,我们的研究证明了在乌克兰战争中由空心子 弹造成的枪伤造成的不同的结肠损伤模式。这种模式包 括较高频率的失血性休克(II期或更高)、CIS II期或 更高,以及结肠壁多发穿孔。所有患者如有腹部穿透伤 (无出口伤口),应怀疑有子弹损伤,必须仔细进行腹 部翻修 为了识别可能的多器官损伤以及肠道的多重枪伤缺陷。 **补充信息** 在线版本包含了补充材料,可在https://doi上获得。org/ 10.1186/s12893-023-01919-6. **额外的fle** **1。表S1。**形状稳定或空心子弹与枪伤原因的关系。 **额外的fle** **2。表S2。**通过形状稳定或空心点子弹定位枪伤缺陷 分析结肠损伤。 **额外的fle** **3。表S3。**用结肠损伤量表分析结肠创伤严重程度与 空心子弹或形状稳定子弹损伤的关系。 **致谢** 不适用。 **作者贡献** KG-研究概念和设计,数据获取;IAL-数据获取,数据分析和解释,文 献检索,手稿起草;IT-数据获取,数据分析和解释;手稿起草,制作 表格和框架;LM-数据获取,数据分析和解释,手稿的起草,文献检索 和分析;Ad监督,研究构思,手稿的关键修改,文件批准。所有的作 者都阅读并批准了fnal的手稿。 **资金** 这项研究没有得到任何资助。 **数据和材料的可用性** 本研究中产生或分析的所有数据均包含在本文中。 **声明** **对参与者的伦理批准和同意** 这项研究是根据《赫尔辛基宣言》进行的。这项研究得到了乌克兰 军事医学院(乌克兰基辅)伦理委员会的批准。被纳入研究的所有 个体参与者均获得了知情同意。 **同意出版** 不适用。 **竞争利益** 作者声明没有任何相互竞争的利益。 **作者详细信息** 1乌克兰武装部队医疗部队司令部,基辅,乌克兰。2军事外科的离开 , 乌克兰军事医学院,基辅,乌克兰。3乌克兰国家医学科学院,基辅 , 乌克兰。4乌克兰基辅, 国家行政部门,国家科学院“预防和临床医 学研究和实践中心 ”。5乌克兰基辅波哥莫莱茨国立医科大学外科,乌 克兰。6基辅国立塔拉斯舍甫琴科大学生物与医学研究所外科外科,德 米夫斯卡13,基辅03039,乌克兰。 收到日期:2023年1月17日 published online:27January2023 古梅纽克等人。*BMC手术* *(2023)* *23:23* 第9页共9 页 **参考文献** 1.沃森JD,亚丁JK,恩格尔杰,拉斯穆森特,格拉斯哥SC。军事结直 肠创伤中结肠造口术的危险因素:867例患者的回顾。手术。 2014;155(6):1052 –61. 2.李赫,孔五世,张C,蒂拉扬五世,拉贾雷特南N,埃尔萨巴赫A, 等。过去十年来腹部枪伤的处理趋势:一个南非的经验。世界J Surg。2022;46(5) :998 – 1005. 3.特塞马四世,贝斯帕连科,迪尼茨,科瓦尔BM,米沙洛夫VG。对当 代战争中导致肢体丧失的破坏性因素的研究。Novosti Khirurgii.2018;26(3):321 –31. 4.史密斯L,本德内利C,李N,里兹MG,罗EJ,Amico F,等。WSES 提供的钝性和穿透性肠损伤指南:诊断、调查和治疗。世界J Emerg Surg。2022;17(1):13. 5.卡兹米尔丘克A、雅尔穆里乌克Y、鲁林I、吉巴罗R、布里亚诺夫O 、德尔卡克S等。乌克兰利用北约的四层“根据需要改变 ”医疗 体系管理战斗伤亡的经验。世界J Surg。2022;46:2858. 6.吉巴罗房车,卢林,萨法诺夫IV,杜德拉迪,奥克雷DV,迪尼茨A。 在乌克兰战争中受伤的战斗病人的胸部和手臂受了枪伤,颈部保 留了子弹:一个病例报告。 国际社会的案件代表。2022;99: 107658. 7.罗戈夫斯基VM,科瓦尔B,卢林IA,古米尼克K,戈罗贝伊科M,迪 尼茨A。在俄乌战争中四肢血管受伤的战斗病人的临时动脉分流 术:一个病例报告。国际社会的案件代表。2022 ;102: 107839. 8.鲁林一世,特塞马四世,古梅尼克K,苏萨克YV,杜本科迪,特 塞马伊。用常规和空心点子弹对石膏上残留伤口腔的实验建模 。乌克兰医学科学(MSU) 。2021;17(4). 9.汉娜,舒伊布,韩特,梅塔,科萨F。火器、子弹和伤口弹道 学:一种成像底漆。受伤。2015;46(7):1186 –96. 10.格拉斯哥特区,老斯蒂尔,邓肯杰,拉斯穆森TE。现代威特菲尔德 结肠直肠创伤的流行病学:对977名联军伤亡人员的回顾。j创伤急 性护理冲浪。2012;73(第6页) :S503-8。 11.O,阿尔谢里夫J,曼索尔S。结肠枪伤:术后并发症发生的预 测危险因素,4年内的经验为172例。ANZ J Surg.2020;90(4):486 –90. 12.古米尼克K,鲁林I,特塞马I,苏萨克Y,米海伦科O, 内霍杜伊科 五世等。利用空心点和形状稳定子弹的弹道塑性线模型上的生物组 织塑性变形的边界弹道学。J Educ健康运动。2021;11(11):37 –57. 13.科门科一世、特塞马一世、赫梅尼克、马卡洛夫、拉胡辛、亚尔里奇 Y等。损伤控制策略和经胆道减压术在肝损伤器官保存手术治疗中 的应用。Mil Med.2022;187(5 –6):e781 –6. 14.史密斯IM,Beech ZK,伦迪JB,鲍利DM。一项关于当代军事手术中 腹部损伤管理的前瞻性观察性研究:损伤控制剖腹手术与高生存 率和低粪便分流率相关。安Surg。2015;261(4):765 –73. 15.王,张,张,徐W,等。穿透性结肠损伤控制手术:吻合术还是造 口?ANZ J Surg.2021;91(9):1874 –80. 16.维尔特雷斯A、韦克菲尔德M、皮克特C、格里尔L、威尔逊A、吉 伦S等。战争相关结肠损伤的一期修复和一期吻合术的结果。J创 伤。2009;66(5):1286 –91. 17.辛巴柳克六世、鲁林、乌森科、古米尼克、克林丘克、格里琴科 等。现代子弹的不同类型和口径的伤口弹道学的实验研究结果 。Med Perspekt.2021;26(4):4 – 14. 18.辛巴柳克六世、鲁林、柴科夫斯基、格拉博维姆、古梅纽克KV 、 内霍杜伊科等。实验中不同类型的子弹对现代柱前炎症性损 伤的组织学结果的比较评价。世界医学生物。2022;1(79):244 –78. 19.我,我,我,我。结肠和直肠的战争损伤-10年后的结果。科尔安 特罗波尔。2002;26(2):441 –6. 20.马尔亚诺维奇,约翰逊,豪森,奥伯迈尔。缺血预处理可提高大鼠 肠吻合口的稳定性。Int J结直肠Dis。2009;24(8):975 –81. 21.等,等,等,等,等,等,等。治疗机制对穿透性结肠创伤的治 疗及预后的影响。我的名字。2018;100(2):152 –6. 22.博塔吉,诺曼,阿尔哈齐,阿特夫。当前也门战争中穿透性结直肠 损伤的一次修复的安全性。亚洲J Res Surg。2022;7(1):8 –22. 23.斯蒂尔SR,沃尔科特KE,穆伦尼克斯PS,马丁MJ,塞贝斯塔JA, 阿扎罗KS,等。伊拉克自由行动中的结肠和直肠损伤:在管理或 结果方面是否有任何变化的趋势?这是结肠直肠。 2007;50(6) :870 –7. 24.费尔克M,奥西波夫R,福斯特K,卡鲁索D,卡西尔A。创伤性结 肠损伤的难题。我J Surg。2004;188(6):663 –70. 25.卡迪M,易 卜拉欣K,阿里扎伊西南,穆罕默德H,加拉蒂M, Rainone A,等。阿富汗拉什卡尔加一家独立的非政府组织医院 中953名腹部穿透伤患者的受伤模式和死亡原因。世界J Emerg Surg。2019 ;14:51. 26.米勒公关,费边TC,克罗马,马格诺蒂LJ,伊丽莎白 ·普里查德F , 米纳德G等。结肠穿透伤后的改善预后:一种临床途径的应用。 安Surg。2002;235(6):775 –81. 27.中超博士,刘易斯先生,斯特里克兰德先生,王志明,黄博士, D。需要切除的破坏性结肠损伤:是否需要进行结肠造口术?j创 伤急性护理冲浪。2022;92:1039. 28.蔡因丁,威廉姆斯,诺涅斯,尼扎姆,奥卢法霍,奥尔特加,等 。美国创伤中心的枪伤:多处枪伤的致命性分析。Am Surg。 2021;87(1):39 –44. **出版商的注意事项** 《施普林格自然》杂志对已出版的地图和机构纠纷中的管辖权主张保持 中立。 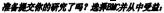 •快速,方便的在线提交 • 由你所在领域中经验丰富的研究人员进行彻底的同行评审 •快速出版《接受》 •支持研究数据,包括大型和复杂的数据类型 •黄金开放获取,促进更广泛的合作和增加的引用 你的研究的最大能见度:每年超过1亿的网站浏览量 在BMC,研究一直在进行中。 学习更多的生物医学中心。com/submissions   Gumeniuk *et al. BMC Surgery (2023) 23:23* <https://doi.org/10.1186/s12893-023-01919-6> BMC Surgery  **RESEARCH Open Access** Gunshot injury to the colon by expanding  eck f update bullets in combat patients wounded in hybrid period of the Russian-Ukrainian war during 2014–2020 Kostiantyn Gumeniuk1,2, Igor A. Lurin3,4, IevgenTsema5, Lesia Malynovska5, Maksym Gorobeiko6 and Andrii Dinets6* **Abstract** **Background** A gunshot wound to the colon is a frequent injury in armed conficts. An example of a high-energy modern weapon is hollow-point bullets, which is associated with increased tissue damage and lethal outcome. The aim of this study was to evaluate gunshot injuries to the colon in combat patients and to assess the diference in clini- cal features of patients with colon injuries by hollow-point versus shape-stable bullets. **Patients and methods** Analyses of clinical data were performed on 374 male soldiers from the Armed Forces of Ukraine with gunshot abdominal wounds with injury to the colon in East Ukraine between 2014 and 2020. Out of 374 injured, 112 (29.9%) patients were diagnosed with penetrating gunshot bullet wounds: 69/112 (61.6%) were injured by shape-stable bullets, and the hollow-point bullets injured 43/112 (38.4%) patients. **Results** More severe hemorrhagic shock stages were inpatients injured by hollow-point bullets: shock stages III-IV was in 25 (58.1%) patients injured by the hollow-point bullets vs. 17 (24.6%) patients injured by shape-stable bullets (p = 0.0004). Left colon parts were more frequently injured as compared to the right colon side or transverse colon: 21 (48.8%) patients were injured by the hollow-point bullets (p < 0.0001), and 41 (59.4%) patients were injured by the shape-stable bullets (p = 0.032). A signifcantdiference was identifed for the frequent injury to the middle colon within the entire cohort (p = 0.023). Patients injured by the hollow-point bullets demonstrated a higher frequency of 3–5 areas of colon gunshot defects, which was detected in 18 (41.8%) patients injured by hollow-point bullets and none with shape-stable bullets injury (p = 0.0001). Colon Injury Scale (CIS) IV was detected in 7 (16.3%) patients injured by the hollow-point bullets as compared to 2 (2.9%) patients injured by shape-stable bullets (p = 0.011). Colostomy was performed in 14 (69%) patients injured by shape-stable bullets and in 12 (27.9%) patients injured by hollow-point bullets (p > 0.05). 15 (35%) patients died after injury by the hollow-point bullet, whereas 9 (13%) patients after damage by the shape-stable bullets (p = 0.0089). **Conclusions** All patients should be suspected to have an injury by bullet with expanding properties in case of penetrating abdominal injury (absent of outlet wound) and careful revision of the abdomen must be performed to identify possible multiorgan injury as well as multiple gunshot defects of the intestine. *Correspondence: Andrii Dinets andrii.dinets@knu.ua Full list of author information is available at the end of the article  BMC © The Author(s) 2023. **Open Access** This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit <http://creativecommons.org/licenses/by/4.0/>. The Creative Commons Public Domain Dedication waiver ([http://creativeco](http://creativecommons.org/publicdomain/zero/1.0/) [mmons.org/publicdomain/zero/1.0/](http://creativecommons.org/publicdomain/zero/1.0/)) applies to the data made available in this article, unless otherwise stated in a credit line to the data. **Keywords** Colon injury, Gunshot, War in Ukraine, Shape-stable bullets, Hollow-point bullet, Expanding bullet **Introduction** A gunshot wound to the colon is a frequent injury in armed conficts, which is associated with severe trauma in combatants due to the increased damage properties of modern high-energy weapons [[1](#bookmark1), [2](#bookmark2)]. Such gunshot inju- ries may cause massive damage to soft tissue and internal organs, resulting in lethal outcomes or more prolonged treatment and rehabilitation time [[3](#bookmark3), [4](#bookmark4)]. Te Russian- Ukrainian war was started in 2014, and for the frst eight years, this war was ongoing as hybrid warfare, followed by the initiation of direct fghts between the two armies in 2022 [[5](#bookmark5), [6](#bookmark6)]. During the hybrid period of 2014–2020, and nowadays, we have noticed Russian army frequently uses various types of weapons with high damage prop- erties (*e.g.* hollow-point bullets), which is prohibited by international law [[7](#bookmark7)]. Considering this fact, military med- ical ofcials in Ukraine came to the question of whether or not the abovementioned types of bullets impact the severity of gunshot wounds and specifc locations of the injuries, as well as relations to the survival of the patients and their treatment. Te results were used to update the clinical guidelines and upgrade military hospitals at the appropriate Level to be ready to provide aid in case of prohibited high-energy weapons, including hollow- point bullets. In this study, we have focused on analyses of colon injury in the abovementioned conditions. Mili- tary medical doctors of Ukraine were challenged with the management and rehabilitation of military personnel who were injured by modern high-energy weapons and received severe abdominal trauma. An example of such a modern weapon is a hollow-point bullet, which is a specially shaped bullet expanding into multiple smaller projectiles upon impacting the target and causing severe injury to soft tissues and internal organs. Te hollow- point bullet could perforate high-class body armor [[8](#bookmark8), [9](#bookmark9)]. Such ballistic properties might be associated with severe abdominal trauma: multiorgan injury, multiple perfora- tions of the bowel with massive fecal diversion, as well as a high risk of bleeding with hemorrhagic shock and retroperitoneal hematomas [[10](#bookmark10), [11](#bookmark11)]. Hollow-point bullet ballistic characteristics are also associated with multiple full-thickness gunshot defects to the colon wall, whereas single defect of the colon wallis uncommon [[8](#bookmark8), [12](#bookmark12)]. Such gunshot trauma with hollow-point bullets could be associated with a lethal outcome to combat patients, even concerning the principle of “golden hour” and dam- age control surgery. Ballistic features of the hollow-point bullets envisage expanding on impact followed by the dis- tribution of multiple fragments or bullet mushrooming, causing more damage to tissues. Using such features, the X-ray became an efective tool for detecting metal frag- ments in the abdomen and establishing the mechanism of injury. Little is known about the gunshot injury to the colon in the warfare in Ukraine. Te aim of this study was to evaluate gunshot injuries to the colon in combat patients and to assess the diference in clinical features of patients with colon injuries by hollow-point versus shape-stable bullets. **Materials and patients** All soldiers from the Armed Forces of Ukraine with gun- shot abdominal trauma and injury to the colon in East Ukraine between 2014 and 2020 were eligible for this retrospective study. In this study, we hypothesize that patients with gunshot injuries to the colon by hollow- point bullets have diferent clinical features and outcomes compared to those injured by shape-stable bullets. Evalu- ation of the patients was performed concerning the bullet types and depended on the presence or absence of frag- mentation hollow-point bullets *vs.* shape-stable bullets. Patients were not included in the study in case of injury by explosive munitions (artillery, land mines, grenades, etc.). Tere were identifed 374 male patients who were surgically treated at a military feld hospital (Level II of medical care) situated in a 20 km zone from the frontline. Te term “Level” is used in the National Military Doc- trine of Ukraine, aiming to show the stratifcation of the fve tiers in which medical aid is provided [[3](#bookmark3), [6](#bookmark6), [7](#bookmark7)]. Each Level is a kind of medical tier to be organized on a pro- gressive basis from 1 to 5 to apply treatment, evacuation, specifc approaches to patient support as well as rehabili- tation. Level I is related to First aid, which is organized during the evacuation or at the point of injury. Level II is corresponded to the military feld hospital with a lim- ited inpatient bed space, functioning within a distance of 20–40 km from the frontline. Laparoscopy is available in hospitals of Level II. Level III is specialized medical and surgical care, which is provided in a large hospital with a bulk of inpatients beds, within a distance of over 40 km from the frontline, in cities like Kharkiv, Dnipro, Odesa, Vinnytsya, Kyiv, where advanced equipment (CT, MRI, etc.) and high-skilled surgeons are available. Level IV is a tier of highly specialized medical aid outside of the bat- tlefeld zone, providing an application of high-tech medi- cal equipment for patients who require more prolonged treatment or who need medical capabilities found inad- equate at lower Level II/III. Level V is a tier of rehabilita- tion facilities. Gumeniuk *et al. BMC Surgery (2023) 23:23* Out of 374 patients with a gunshot injury to the colon, 112 (29.9%) patients with penetrating bul- let wounds comprised the study group, whereas 262 (70.1%) patients were not included in the because of penetrating gunshot wounds due to shrapnel injury. Out of 112 patients from the study group, 69 (61.6%) were injured by shape-stable bullets, and hollow- point bullets injured 43 (38.4%) patients. Evacuation of injured patients from the battlefield was performed within the “golden hour” [[13](#bookmark13)]. All patients received medical aid at Level II. At admission to Level II hospital, all patients were diag- nosed with gunshot injuries and hemorrhagic shock requiring resuscitation at the intensive care unit (ICU). Shock severity was determined according to the Amer- ican College of Surgeons Advanced Trauma Life Sup- port (ATLS). Damage control tactics was applied to all patients. Injury to the colon was evaluated according to the Colon Injury Scale (CIS). Computed tomography was not available at Level II. Abdominal X-ray was applied to detect the localiza- tion of the projectile or its fragments orientation (tum- bling), deformation, and fragmentation (number of fragments and area of fragments dissemination). Right colon parts constituted cecum, ascending colon, and hepatic flexure. Left colon parts formed splenic colon flexure, descending, and sigmoid colon. As upper colon, we considered the transverse colon, hepatic and splenic flexures, middle colon—ascending and descending colon, and lower colon—cecum and sigmoid colon. **Statistical analyses** Statistical analyses were performed using the software SPSS v.22 (IBM, USA). A chi-squared test (χ2-test) was applied to test the null hypothesis for categorical val- ues, whereas Student’s t-test and One-way analysis of variance were used for continuous variables. Statistical difference was considered as significant at p < 0.05. Page 3 of 9 **Results** Te mean age of all patients was 24.7 years (range 19–47 years). 82 (73.2%) patients were evacuated within the 1 h (mean time 55.3 ± 1.17 min) from the moment of injury until the admission to Level II, which is inline with the principle of “golden hour.” Data analyses are presented in the Tables. Detailed statistical data are shown in Additional fle [1](#bookmark14): Table S1, Additional fle [2](#bookmark15): Table S2, Additional fle [3](#bookmark16): Table S3. Analyses of hemorrhagic shock stages are presented in Table [1](#bookmark17) and Additional fle [1](#bookmark14): Table S1. A hemorrhagic shock Stage III was diagnosed in 18 (41.9%) patients injured by the hollow-point bullets, which is more fre- quent as compared to 13 (18.8%) patients injured by shape-stable bullets (p = 0.0081). In contrast, hemor- rhagic shock Stage I was diagnosed in 2 (4.7%) patients injured by the hollow-point bullets, which were less frequent as compared to 25 (36.2%) patients injured by shape-stable bullets (p = 0.0001). Shock Stages I-II were detected in 52 (75.4%) patients injured by shape-stable bullets as compared to 18 (41.9%) patients injured by hol- low-point bullets (p = 0.0004). At laparotomy or laparoscopy, all 112 (100%) patients were diagnosed with various localization of damages to the colon wall (Table [2](#bookmark18), Figs. [1](#bookmark19), [2](#bookmark20)). Data analyses showed that left colon parts were more frequently injured as compared to right colon or transverse colon in 21 (48.8%) injured by the hollow-point bullets (p < 0.0001) and in 41 (59.4%) patients injured by the shape-stable bullets. Data analyses showed that 80 (71.4%) patients were diagnosed with a gunshot injury to the left side and middle colon. Analyses of the entire cohort showed multiple inju- ries to the colon in 65 (58%) patients, whereas a single colon gunshot wound was detected in 47 (42%) patients (Table [3](#bookmark21)). All 43 (100%) patients injured by hollow-point bullet injury had multiple wounds to the colon (2 or more defects), which is 3 times more frequent as com- pared to 22 (31.8%) patients injured by shape-stable bullets with borderline signifcance (p = 0.0488). Also, 18 (41.8%) patients injured by the hollow-point bullets demonstrated a higher frequency of 3–5 defects of the **Table 1** Analyses of the hemorrhagic shock severity in relation to cause of gunshot injury by shape-stable or hollow-point bullets **Shock severity** **Grouping of patients** **All patients n** = **112** **p value** **Injured by Shape-stable bullets n** = **69** **Injured by Hollow-point bullets n** = **43** Stages I 25 (36.2%) 2 (4.7%) 27 (24.1%) 0.0001 II 27 (39.1%) 16 (37.2%) 43 (38.4%) 0.8389 III 13 (18.8%) 18 (41.9%) 31 (27.7%) 0.0081 IV 4 (5.8%) 7 (16.3%) 11 (9.8%) 0.0699 Gumeniuk *et al. BMC Surgery (2023) 23:23* Page 4 of 9 **Table 2** Analyses of colon injury by localizations of gunshot defects by shape-stable or hollow-point bullets **Colon parameters** **Grouping of patients** **All patients n** = **112** **p value** **Injured by Shape-stable bullets n** = **69** **Injured by Hollow-point bullets n** = **43** Colon part Cecum 6 (8.7%) 2 (4.7%) Ascending colon 9 (13.0%) 9 (20.9%) 18 (16.1%) 0.27 Hepatic fexure 3 (4.3%) 4 (9.3%) 7 (6.3%) 0.29 Transverse colon 10 (14.5%) 7 (16.3%) 17 (15.2%) 0.80 Splenicfexure 5 (7.2%) 1 (2.3%) 6 (5.4%) 0.26 Descending colon 21 (30.4%) 12 (27.9%) 33 (29.5%) 0.78 Sigmoid colon 15 (21.7%) 8 (18.6%) 23 (20.5%) 0.69 p-value—comparisons within each group Colon side 0.0005 0.0171 < 0.0001 Right-side colon 18 (26.1%) 15 (34.9%) 33 (29.5%) 0.32 Transverse colon 10 (14.5%) 7 (16.3%) 17 (15.2%) 0.80 Left-side colon 41 (59.4%) 21 (48.8%) 62 (55.4%) 0.27 p-value—comparisons within each group Colon level < 0.0001 0.032 < 0.0001 Upper colon 18 (26.1%) 12 (27.9%) 30 (26.8%) 0.83 Middle colon 30 (43.5%) 21 (48.8%) 51 (45.5%) 0.58 Lower colon 21 (30.4%) 10 (23.3%) 31 (27.7%) 0.41 p-value—comparisons within each group Relation to peritoneum 0.18 0.091 0.023 Intraperitoneal 39 (56.5%) 22 (51.2%) 61 (54.5%) 0.58 Extraperitoneal 30 (43.5%) 21 (48.8%) 51 (45.5%) p-value—comparisons within each group 0.44 0.91 0.50 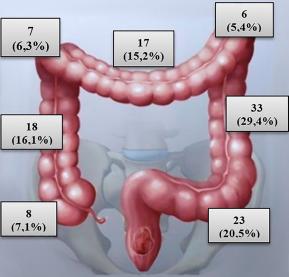 **Fig. 1** Schematic illustration of gunshot injury to the various parts of the colon of study cohort colon wall, compared to the absence of the patients with shape-stable bullets injury (p = 0.0001). Wounds to the colon with ≥ 5 defects of the colon wall were identifed in 4 (9.3%) patients injured by the hollow-point bullets, but none of the patients with shape-stable bullets injury (p = 0.0199). CIS analyses are reported in Table [4](#bookmark22) and Additional fle [3](#bookmark16): Table S3. A signifcantly higher frequency of CIS III was detected in 11 (25.6%) patients injured by the hollow- point bullets as compared to 7 (10.1%) patients injured by shape-stable bullets (p = 0.031). CIS IV was detected in 7 (16.3%) patients injured by the hollow-point bullets as compared to 2 (2.9%) patients injured by shape-stable bullets (p = 0.011). X-ray showed foreign metal density objects in the abdomen in 17 (24.6%) patients injured by shape-stable bullets, which was subsequently confrmed at laparotomy (Fig. [3](#bookmark23)). In 12 (27.9%) patients injured by hollow-point bullets were found various sizes of multiple bullet frag- ments in the quantity of up to 5 fragments in 7 (16.3%) patients, 6 to 10 fragments in 13 (30.2%) patients, and 11–15 fragments in 11 (25.6%) patients. Abdomen X-ray examples of bullet fragments are illustrated in Fig. [3](#bookmark23). Gumeniuk *et al. BMC Surgery (2023) 23:23* Page 5 of 9 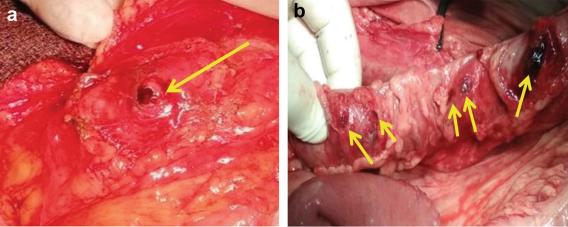 **Fig. 2** Intraoperative photograph of colon gunshot injury. **A** A single wound to the colon (entry gunshot hole marked with an arrow). **B** Multiple injuries to the colon by fragments of bullet (marked with arrows) **Table 3** Analyses of colon injury by localizations and number of gunshot defects by shape-stable or hollow-point bullets **Colon injury location** **Grouping of patients** **Injured by Shape-stable bullets n** = **69** **2 3–4** ≥ **5** **Injured by Hollow-point bullets n** = **43** **Number of colon defects, n** = **2 3–4** ≥ **5** Cecum, n = 0 0 0 1 1 0 Ascending colon, n = 3 0 0 5 4 0 Hepatic fexure, n = 2 0 0 3 1 0 Transverse colon, n = 1 0 0 2 4 1 Splenicfexure, n = 3 0 0 0 1 0 Descending colon, n = 4 0 0 7 3 2 Sigmoid colon, n = 9 0 0 3 4 1 Total 22* (31.8%) 0 0 21 (48.8%) 18 (41.8%)** 4 (9.3%)*** p-value: *0.0488, **0.0001, ***0.0199 **Table 4** Analyses of colon trauma severity by Colon Injury Scale in relation to hollow-point bullets or shape-stable bullets injury **Colon Injury Scale (CIS) parameters** **Grouping of patients** **All wounded n** = **112** **p value** **Injured by Shape-stable bullets n** = **69** **Injured by Hollow-point bullets n** = **43** CIS stage I 28 (40.6%) 0 (0.0%) 28 (25.0%) < 0.0001 II 31 (44.9%) 23 (53.5%) 54 (48.2%) 0.38 III 7 (10.1%) 11 (25.6%) 18 (16.1%) 0.031 IV 2 (2.9%) 7 (16.3%) 9 (8.0%) 0.011 V 1 (1.4%) 2 (4.7%) 3 (2.7%) 0.31 Mushrooming bullets (Fig. [4](#bookmark24)) were identifed in 19 (44.2%) patients injured by hollow-point bullets and in no patients injured by shape-stable bullets (p < 0.0001). Te list of operations is summarized in Table [5](#bookmark25). Tere was no signifcant diference in the types of operations in the study groups. Colostomy was performed in 14 (20.3%) patients injured by shape-stable bullets and 12 (27.9%) patients injured by hollow-point bullets. Postoperative death was observed in 24 (21.4%) patients. Of these, 15 (35%) patients died after injury by the Gumeniuk *et al. BMC Surgery (2023) 23:23* Page 6 of 9 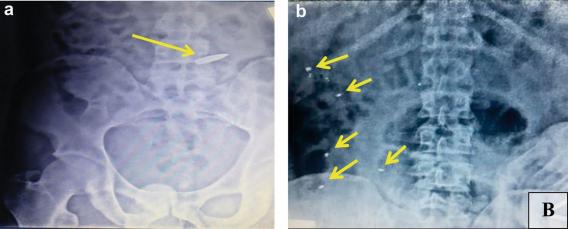 **Fig. 3** Photographs of X-ray flms illustrating intraabdominal fragments with metal density features  **Fig. 4** Intraoperative photograph demonstrating hollow-point bullet with mushrooming efect (a yellowish metal object in the arms of the surgeon) hollow-point bullet, whereas 9 (13%) patients after damage by the shape-stable bullets (p =0.0089). Causes of mortality at Level II were massive hemorrhage, heart and respiratory failures. Causes of mortality at Level III were the failure of colorectal anastomoses and anastomotic leak, peritonitis, and perforated peptic ulcer of the small intestine. Causes of mortality at Level IV were sepsis, abdominal abscesses, purulent pneumonia, and acute bowel obstruction. Detailed follow-up data is unavailable, which is a limitation. **Discussion** Tis paper is the frst study reporting data from a combat cohort with injury to the colon by hollow-point bullets, which have been used against Ukrainian Armed Forces since 2014. War in Ukraine is associated with specifc patterns of colon injuries due to the application of pro- hibited weapons, including hollow-point pullets, against Ukrainian Armed Forces. Such violation of international war-related law was not described previously in the lit- erature. Although NATO standards are routinely applied for individual body protection by using the tactical hel- met and modular tactical vest for the ballistic protection of the neck, chest, abdomen, and groin, our results show severe colon injury. Te research is ongoing to develop better individual body protection, considering the dam- age properties of modifed bullets, but details of such research are classifed and unavailable. Tis study high- lighted various clinical outcomes of colon injury in case of damage by modern hollow-point bullets as compared to conventional types of shape-stable bullets. Tis study showed severe trauma and a higher mortality rate for patients injured by hollow-point bullets. Our fndings shed light on clinical features and management of gun- shot colon injury, which might be helpful in further clini- cal application for both civil and combat casualties. Similar to other reports, we showed that most patients were evacuated within the “golden hour” to Level II and treated according to the principle of damage control sur- gery. Damage control surgery is a standard protocol for Ukrainian military medicine and is in line with other studies of abdominal gunshot trauma [[13](#bookmark13)–[16](#bookmark26)]. Although we have not found publications with a spe- cifc reference to the hollow-point bullet injury *vs.* shape- stable bullets, evidence from this study, as well as other experimental studies of internal wound ballistics, con- frms our data concerning increased tissue damage by such kind of weapon [[8](#bookmark8), [9](#bookmark9), [17](#bookmark27), [18](#bookmark28)]. Our fndings demon- strate that most patients had concurrent damage to other organs, supporting the abovementioned hypothesis. Gumeniuk *et al. BMC Surgery (2023) 23:23* Page 7 of 9 **Table 5** Analyses of surgical operation in study cohort **Operation type** **Injured by shape-** **stable bullets n** = **69** **Injured by hollow- point bullets** **n** = **43** Laparoscopiccolon wound primary repair, n = 2 (3.0%) 0 Colon wound primary repair, n = 3 (4.3%) 0 Colon wound primary repair + colostomy, n = 0 1 (2.3%) Colon wound primary repair + small intestine resection, n = 21 (30.4%) 9 (20.9%) Colon wound primary repair + colostomy + ureter wound primary repair and ureter stenting, n = 0 2 (4.6%) Colon wound primary repair + cholecystectomy, n = 3 (4.3%) 0 Colon wound primary repair, transversostomy + stomach wound primary repair, n = 4 (5.8%) 2 (4.6%) Colon wound primary repair + splenectomy, n = 2 (3.0%) 2 (4.6%) Colon wound primary repair + liver wound primary repair + colostomy, n = 3 (4.3%) 2 (4.6%) Colon wound primary repair + colostomy + pancreatic wound primary repair, n = 2 (3.0%) 0 Extraperitonization, n = 2 (3.0%) 0 Right hemicolectomy, n = 2 (3.0%) 2 (4.6%) Right hemicolectomy + ileostomy, n = 0 1 (2.3%) Right hemicolectomy + right nephrectomy, n = 2 (3.0%) 5 (11.6%) Right hemicolectomy + liver wound primary repair, n = 14 (20.0%) 5 (11.6%) Left hemicolectomy, n = 1 (1.4%) 0 Left hemicolectomy + left nephrectomy, n = 3 (4.3%) 8 (18.6%) Hartmann’s operation, n = 1 (1.4%) 2 (4.6%) Hartmann’s operation + bladder wound primary repair, n = 4 (5.8%) 2 (4.6%) Inline with Busić et al. and Elfaedy et al., we also dem- onstrated a high incidence of hemorrhagic shock in our patients, suggesting such gunshot complications as a common event [[11](#bookmark11), [19](#bookmark29)]. Also, we have shown a higher frequency of hemorrhagic shock in patients injured by hollow-point than shape-stable bullets, which is another evidence of severe trauma from the modern weapon. Te higher severity of shock is associated with higher levels of ischemia and necrosis of colon tissues, which act to increase bacterial colonization, resulting in a higher risk for anastomosis leak or failure [[11](#bookmark11), [20](#bookmark30)]. Similar to other reports, the left colon part (*i.e.,* splenic colon fexure, descending and sigmoid colon) and middle colon (ascending and descending colon) were frequently injured as compared to other sites [[1](#bookmark1), [11](#bookmark11), [21](#bookmark31)–[24](#bookmark32)]. Te importance to note that colon injury is related to a higher risk of fecal diversion. Watson et al. showed the high risk of fecal diversion in combat patients with left-side colon injury by high-energy projectiles. Our fndings also dem- onstrate a high frequency of left-side colon injury, and we hypothesize that patients with such locations of gunshot wounds have a higher risk for complications and need to undergo a colostomy. However, we also suggest con- sidering the bullet type (*i.e.,* the hollow-point bullet) as an additional factor to increase tissue damage. Our fnd- ings would seem to suggest that mechanisms of injury by modern bullets may afectall colon parts without relation to bullet type. Unlike other research carried out in this area, we showed multiple injuries to the colon in 58% of patients, which is higher compared to other cohorts. For exam- ple, Oosthuizen et al. showed 12% and Steele et al. 15% of multiple injuries in patients diagnosed with more than one injury to the colon in the study of non-combat trauma [[21](#bookmark31), [23](#bookmark33)]. Cardi et al. demonstrated multiple seg- ment injuries in both large and small bowel in 21.3% of the patients [[25](#bookmark34)]. However, our fnding aligns with Bothaigi et al., who showed 64 colorectal wounds in 56 patients in the study of abdominal battlefeld trauma [[22](#bookmark35)]. Tese diferences can be explained by the frequent appli- cation of the hollow-point bullets in our cohort com- pared to others. Analyses of CIS showed that 48.2% of patients had CIS II or greater in the entire cohort. Our observation is con- sistent with Fealk et al., reporting 59% of patients to have CIS > 2 as well as with Miller et al., who showed a mean CIS of 2.4 [[24](#bookmark32), [26](#bookmark36)]. In this study, we showed no patients to have CIS I but a higher frequency of CIS III and IV among individuals injured by the hollow-point bullets compared to shape-stable bullets. Tese fndings could potentially play a signifcant role in management of the patients injured with expanding bullets as well as provide Gumeniuk *et al. BMC Surgery (2023) 23:23* an evidence of expanding bullets to cause severe colon trauma. Te overall rate of colostomy in our cohort (20.3%) is in contrast to other reports: Steele (33%), Glasgow (36.3%), Watson (36.9%), Oosthuizen et al. (50%) or Mitchao etal. (2.5%) [[1](#bookmark1), [10](#bookmark10), [15](#bookmark37), [23](#bookmark33), [27](#bookmark38)]. Cardi et al. showed colostomies in 13.6% of the patients with colorectal wounds in case of high fecal spread or at damage control surgery [[25](#bookmark34)]. As judged from the analyses of other series and our experi- ence, there are multiple factors to play a role in surgeons’ decision to choose a certain operative approach in each situation, including a colostomy. Te observed propor- tion of colostomies could be attributed to severe colon trauma, which is in line with the previously published series [[15](#bookmark37), [16](#bookmark26), [21](#bookmark31)]. We agree with other researchers sug- gesting avoiding colostomy and performing primary closure in selected injured patients by shape-stable bul- lets [[15](#bookmark37), [16](#bookmark26), [21](#bookmark31)]. However, in this study, colon injury by the hollow-point bullets is associated with more severe trauma, and the decision to perform a colostomy should be made after the evaluation of the abdomen in the con- text of damage control surgery. Mortality is usually high in patients with gunshot colon wounds, mainly because of multiorgan injury and severe hemorrhagic shock [[15](#bookmark37)]. In our study, we showed lethal outcomes in 21.4% of patients, which is close to data in studies of Oosthuizen et al., who showed overall mor- tality of 26%, and Vertrees et al. 29% of patients with gunshot wounds [[11](#bookmark11), [16](#bookmark26)]. In contrast, Elfaedy et al. dem- onstrated mortality of 6.9%; however, in that study, 40% of patients were not in hemorrhagic shock, which is a risk factor for death in patients with an abdominal gunshot injury, including colon [[11](#bookmark11)]. Glasgow et al. showed overall mortality of 9.5% [[10](#bookmark10)]. Steel etal. showed 17.7% mortality in combat patients [[23](#bookmark33)]. Zero colon-related mortality was demonstrated by Bothaigi et al. and Mitchao et al. [[22](#bookmark35), [27](#bookmark38)]. Cardi et al. showed a mortality of 12.8%, with hem- orrhagic shock as the most frequent cause of death [[25](#bookmark34)]. According to the published series, mortality is reported to be high in multiple gunshot wounds, as also shown in this study [[28](#bookmark39)]. **Conclusions** To sum up, our study demonstrated diferent colon injury patterns due to gunshot wounds by the hollow-point bullets in the war in Ukraine. Tese patterns include a higher frequency of hemorrhagic shock (stage II or higher), CIS II or higher, as well as multiple perforations of colon walls. All patients should be suspected to have an injury by bullet with expanding properties in case of penetrating abdominal injury (absent of outlet wound) and careful revision of the abdomen must be performed Page 8 of 9 to identify possible multiorgan injury as well as multiple gunshot defects of the intestine. **Supplementary Information** The online version contains supplementary material available at [https://doi.](https://doi.org/10.1186/s12893-023-01919-6) [org/10.1186/s12893-023-01919-6](https://doi.org/10.1186/s12893-023-01919-6). **Additional fle 1. Table S1.** Analyses of the hemorrhagic shock severity in relation to cause of gunshot injury by shape-stable or hollow-point bullets. **Additional fle 2. Table S2.** Analyses of colon injury by localizations of gunshot defects by shape-stable or hollow-point bullets. **Additional fle 3. Table S3.** Analyses of colon trauma severity by Colon Injury Scale in relation to hollow-point bullets or shape-stable bullets injury. **Acknowledgements** Not applicable. **Author contributions** KG—study conception and design, acquisition of data; IAL—acquisition of data, analysis and interpretation of data, literature search, drafting of the manuscript; IT—acquisition of data, analysis and interpretation of data; draft- ing of the manuscript, making tables and fgures; LM—acquisition of data, analysis and interpretation of data; MG—analysis and interpretation of data, drafting of manuscript, literature search and analyses; AD—supervision, study conception, critical revision of the manuscript,fnal approval. All authors read and approved the fnal manuscript. **Funding** This study received no funding. **Availability of data and materials** All data generated or analyzed during this study are included in this published article. **Declarations** **Ethics approval and consent to participant** The study was performed in accordance with the Declaration of Helsinki. This study was approved by the Ethical Committee at the Ukrainian Military Medical Academy (Kyiv, Ukraine). Informed consent was obtained from all individual participants included in the study. **Consent for publication** Not applicable. **Competing interests** The authors declare no competing interests. **Author details** 1 Medical Forces Command, Armed Forces of Ukraine, Kyiv, Ukraine. 2 Depart- ment of Military Surgery, Ukrainian Military Medical Academy, Kyiv, Ukraine. 3 National Academy of Medical Sciences of Ukraine, Kyiv, Ukraine. 4State Institution of Science“Research and Practical Center of Preventive and Clini- cal Medicine”, State Administrative Department, Kyiv, Ukraine. 5 Department of Surgery, Bogomolets National Medical University, Kyiv, Ukraine. 6 Depart- ment of Surgery, Institute of Biology and Medicine, Taras Shevchenko National University of Kyiv, Demiїvska 13, Kyiv 03039, Ukraine. Received: 25 September 2022 Accepted: 17 January 2023 published online:27January2023 Gumeniuk *et al. BMC Surgery (2023) 23:23* Page 9 of 9 **References** 1. Watson JD, Aden JK, Engel JE, Rasmussen TE, Glasgow SC. Risk factors for colostomy in military colorectal trauma: a review of 867 patients. Surgery. 2014;155(6):1052–61. 2. Lee H, Kong V, Cheung C, Thirayan V, Rajaretnam N, Elsabagh A, et al. Trends in the management of abdominal gunshot wounds over the last decade: a South African experience. World J Surg. 2022;46(5):998–1005. 3. Tsema IV, Bespalenko AA, Dinets AV, Koval BM, Mishalov VG. Study of damaging factors of contemporary war, leading to the limb loss. Novosti Khirurgii. 2018;26(3):321–31. 4. Smyth L, Bendinelli C, Lee N, Reeds MG, Loh EJ, Amico F, et al. WSES guidelines on blunt and penetrating bowel injury: diagnosis, investiga- tions, and treatment. World J Emerg Surg. 2022;17(1):13. 5. Kazmirchuk A, Yarmoliuk Y, LurinI, Gybalo R, Burianov O, DerkachS, et al. Ukraine’s experience with management of combat casualties using NATO’s Four-Tier “Changing as Needed” healthcare system. World J Surg. 2022;46:2858. 6. Gybalo RV, Lurin IA, Safonov V, Dudla DI, Oklei DV, Dinets A. Retained bulletin the neck after gunshot wounds to the chest and arm in combat patient injured in the war in Ukraine: a case report. IntJ Surg Case Rep. 2022;99: 107658. 7. RogovskyiVM, Koval B, Lurin IA, Gumeniuk K, Gorobeiko M, Dinets A. Temporary arterialshunts in combat patient with vascular injuries to extremities wounded in Russian-Ukrainian war: a case report. IntJ Surg Case Rep. 2022;102: 107839. 8. LurinI, Tsema IV, Gumenuik K, SusakYV, Dubenko DY, Tsema YI. Experi- mental modeling of a residual wound cavity on a balistic plasticine using conventional and hollow point bullets. Med Sci Ukraine (MSU). 2021;17(4). 9. Hanna TN, ShuaibW, Han T, Mehta A, Khosa F. Firearms, bullets, and wound ballistics: an imaging primer. Injury. 2015;46(7):1186–96. 10. Glasgow SC, SteeleSR, Duncan JE, Rasmussen TE. Epidemiology of modern battlefeld colorectal trauma: a review of 977 coalition casualties. J Trauma Acute Care Surg. 2012;73(6 Suppl 5):S503–8. 11. Elfaedy O, Elgazwi K, Alsharif J, Mansor S. Gunshot wounds to the colon: predictive risk factors for the development of postoperative complications, an experience of 172 cases in 4 years. ANZ J Surg. 2020;90(4):486–90. 12. Gumeniuk K, LurinI, Tsema I, SusakY, Mykhaylenko O, Nehoduiko V, et al. Woundary ballistics of biological tissue’s plastic deformation on the model of ballistic plastiline using hollow point and shape-stable bullets. J Educ Health Sport. 2021;11(11):37–57. 13. Khomenko I, Tsema I, Humeniuk K, Makarov H, Rahushyn D, Yarynych Y, et al. Application of damage control tactics and transpapillary biliary decompression for organ-preserving surgical management of liver injury in combat patient. Mil Med. 2022;187(5–6):e781–6. 14. Smith IM, Beech ZK, Lundy JB, Bowley DM. A prospective observational study of abdominal injury management in contemporary military opera- tions: damage control laparotomy is associated with high survivability and low rates of fecal diversion. Ann Surg. 2015;261(4):765–73. 15. Oosthuizen G, BuitendagJ, Variawa S, ČačalaS, Kong V, Xu W, et al. Penetrating colonic trauma and damage control surgery: anastomosis or stoma? ANZ J Surg. 2021;91(9):1874–80. 16. Vertrees A, Wakefeld M, Pickett C, Greer L, Wilson A, Gillern S, et al. Out- comes of primary repair and primary anastomosis in war-related colon injuries. J Trauma. 2009;66(5):1286–91. 17. Tsymbalyuk VI, Lurin IA, Usenko OY, Gumeniuk KV, KrymchukSG, Gryshchenko OV, et al. Results of experimental research of wound bal- listics of separate types and calibers of modern bullets. Med Perspekt. 2021;26(4):4–14. 18. Tsymbalyuk VI, Lurin IA, Chaikovskyi YB, GraboviyOM, Gumenyuk KV, Nehoduiko VV, et al. Comparative evaluation of histological results of modern fre infammatory injuries of the column by diferent types of bullets in the experiment. World Med Biol. 2022;1(79):244–78. 19. Busić Z, Rudman F, Stipancić I, Amić E, Busić D. War injuries of colon and rectum–results after 10 years. Coll Antropol. 2002;26(2):441–6. 20. MarjanovicG, Jüttner E, Zur Hausen A, Theodor Hopt U, Obermaier R. Ischemic preconditioning improves stability of intestinal anastomoses in rats. IntJ Colorectal Dis. 2009;24(8):975–81. 21. Oosthuizen GV, Kong VY, Estherhuizen T, Bruce JL, Laing GL, Odendaal JJ, et al. The impact of mechanism on the management and outcome of penetrating colonic trauma. Ann R Coll Surg Engl. 2018;100(2):152–6. 22. Al BothaigiSS, Al Fakih SA, NomanTA, AlharaziT, AtefTA. Safety of primary repair in penetrating colorectal injuries during current Yemeni War. Asian J Res Surg. 2022;7(1):8–22. 23. Steele SR, Wolcott KE, Mullenix PS, Martin MJ, SebestaJA, Azarow KS, et al. Colon and rectal injuries during Operation Iraqi Freedom: are there any changing trends in management or outcome? Dis Colon Rectum. 2007;50(6):870–7. 24. FealkM, Osipov R, Foster K, Caruso D, Kassir A. The conundrum of trau- matic colon injury. Am J Surg. 2004;188(6):663–70. 25. Cardi M, Ibrahim K, Alizai SW, Mohammad H, Garatti M, Rainone A, et al. Injury patterns and causes of death in 953 patients with penetrating abdominal war wounds in a civilian independent non-governmental organization hospital in Lashkargah, Afghanistan. World J Emerg Surg. 2019;14:51. 26. Miller PR, Fabian TC, Croce MA, Magnotti LJ, Elizabeth Pritchard F, Minard G, et al. Improving outcomes following penetrating colon wounds: appli- cation of a clinical pathway. Ann Surg. 2002;235(6):775–81. 27. Mitchao DP, Lewis MR, Strickland M, Benjamin ER, Wong MD, Demetria- des D. Destructive colon injuries requiring resection: is colostomy ever indicated?J Trauma Acute Care Surg. 2022;92:1039. 28. ZeineddinA, Williams M, Nonez H, Nizam W, Olufajo OA, Ortega G, et al. Gunshot injuries in American trauma centers: analysis of the lethality of multiple gunshot wounds. Am Surg. 2021;87(1):39–44. **Publisher’s Note** Springer Nature remains neutral with regard to jurisdictional claims in pub- lished maps and institutional afliations. ***Ready to submityour research? Choose BMC andbenefitfrom:*** **•** fast, convenient online submission **•** thorough peer review by experienced researchers in your field **•** rapid publication on acceptance **•** support for research data, including large and complex data types **•** gold Open Access which fosters wider collaboration and increased citations **•** maximum visibility for your research: over 100M website views per year **At BMC, research is always in progress.** **Learn more** biomedcentral.com/submissions  BMC
nyp366888891
2024年12月9日 14:17
转发文档
收藏文档
上一篇
下一篇
手机扫码
复制链接
手机扫一扫转发分享
复制链接
Markdown文件
HTML文件
PDF文档(打印)
分享
链接
类型
密码
更新密码